Foot & Ankle Injuries
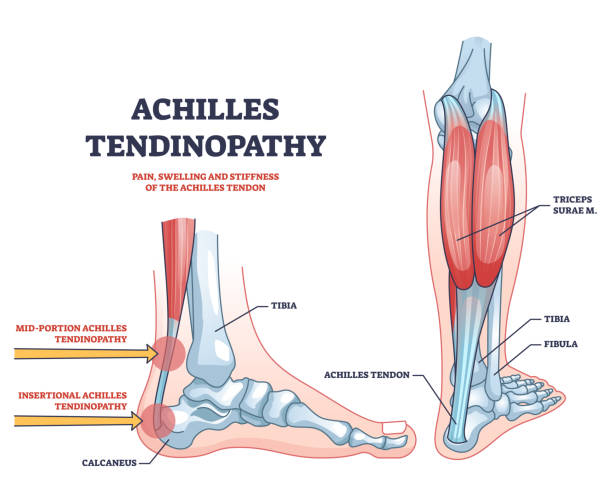
Achilles Tendonitis
The achilles tendon attaches the muscles of the posterior calf to the calcaneus. The Achilles tendon does not have good blood supply or cell activity, so this injury can be slow to heal. The tendon receives nutrients from the tendon sheath or paratendon.
When an injury occurs to the tendon, cells from surrounding structures migrate into the tendon to assist in repair. Some of these cells come from blood vessels that enter the tendon to provide direct blood flow to increase healing. With the blood vessels come nerve fibers. Researchers including Alfredson and his team in Sweden [1] believe these nerve fibers to be the cause of the pain – they injected local anaesthetic around the vessels and this decreased significantly the pain from the Achilles tendon.

Causes & Treatment
Achilles tendonosis is a classic overuse sydrome. Most lower extremity injuries are caused by overuse, and typically occur with a change in shoes, surface, or intensity. Examples would be increasing speed or mileage too quickly for a runner, changing types, styles, or shoe companies, and changing from a treadmill to outdoor surfaces. These variables can all alter biomechanics of the knee and ankle joints. Growth spurts while athletes are maturing, can also alter the mechanics enough to cause one of the above conditions. Athletes transitioning too quickly to barefoot or minimalist shoes, can also easily instigate an achilles tendonosis episode, due to the increase of flexibility required to run without a raised heel running shoe.
In our office, we treat achilles tendonosis with a combination of Active Release Techniques and Graston Technique, along with eccentric stretching and ultimately a strength and stabilization program for surrounding anatomy.
Related Articles:
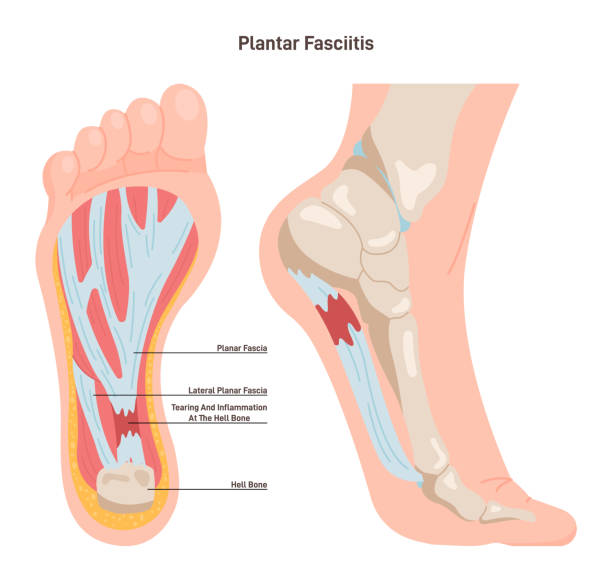
Plantar Fascia
Plantar fasciitis (PF) is a painful inflammatory process of the plantar fascia, the connective tissue on the sole (bottom surface) of the foot. It is often caused by overuse of the plantar fascia or arch tendon of the foot. It is a very common condition and can be difficult to treat if not looked after properly. Another common term for the affliction is “policeman’s heel”.[1]
Longstanding cases of plantar fasciitis often demonstrate more degenerative changes than inflammatory changes, in which case they are termed plantar fasciosis.[2] The suffix “osis” implies a pathology of chronic degeneration without inflammation. Since tendons and ligaments do not contain blood vessels, they do not actually become inflamed. Instead, injury to the tendon is usually the result of an accumulation over time of microscopic tears at the cellular level.
The plantar fascia is a thick fibrous band of connective tissue originating on the bottom surface of the calcaneus (heel bone) and extending along the sole of the foot towards the toes. It has been reported that plantar fasciitis occurs in two million Americans a year and in 10% of the U.S. population over a lifetime.[3] It is commonly associated with long periods of weight bearing. Among non-athletic populations, it is associated with a high body mass index.[4] The pain is usually felt on the underside of the heel and is often most intense with the first steps of the day. Another symptom is that the sufferer has difficulty bending the foot so that the toes are brought toward the shin (decreased dorsiflexion of the ankle). A symptom commonly recognized among sufferers of plantar fasciitis is an increased probability of knee pains, especially among runners.

Causes & Treatment
Most lower extremity injuries are caused by overuse, and typically occur with a change in shoes, surface, or intensity. Examples would be increasing speed or mileage too quickly for a runner, changing types, styles, or shoe companies, and changing from a treadmill to outdoor surfaces. These variables can all alter biomechanics of the knee and ankle joints. Growth spurts while athletes are maturing, can also alter the mechanics enough to cause one of the above conditions. Athletes transitioning too quickly to barefoot or minimalist shoes, can also easily instigate an episode of plantar fasciaitis, due to the increase of flexibility required to run without a raised heel running shoe.
Our office treats plantar fascia with a combination of Active Release Techniques, Graston techniques, and sport taping to reinforce the anatomy, this combined with stretching, cryokinetics, and ultimately strength and stabilization of the surrounding anatomy get us results where others fail.
Related Articles:
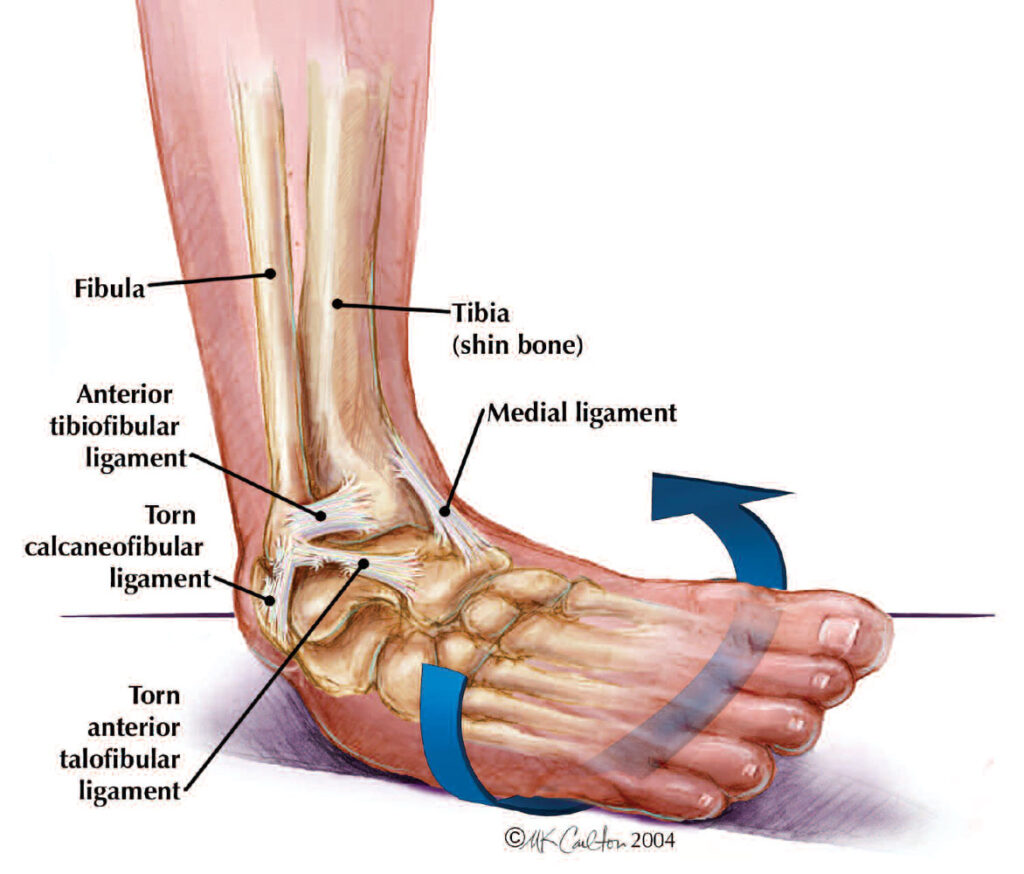
Ankle Sprain
(wikepedia)
Movements – especially twisting, turning, and rolling of the foot – are the primary cause of an ankle sprain.[2] The risk of a sprain is greatest during activities that involve explosive side-to-side motion, such as tennis or basketball. Sprained ankles can also occur during normal daily activities such as stepping off a curb or slipping on ice. Returning to activity before the ligaments have fully healed may cause them to heal in a stretched position, resulting in less stability at the ankle joint. This can lead to a condition known as Chronic Ankle Instability (CAI), and an increased risk of ankle sprains.
The following factors can contribute to an increased risk of ankle sprains:
Weak muscles/tendons that cross the ankle joint, especially the muscles of the lower leg that cross the outside, or lateral aspect of the ankle joint (i.e. peroneal or fibular muscles);
Weak or lax ligaments that join together the bones of the ankle joint – this can be hereditary or due to overstretching of ligaments as a result of repetitive ankle sprains;
Poor ankle flexibility;[citation needed]
Lack of warm-up and/or stretching before activity;[citation needed]
Inadequate joint proprioception (i.e. sense of joint position);
Slow neuron muscular response to an off-balance position;
Running on uneven surfaces;
Shoes with inadequate heel support; and
Wearing high-heeled shoes – due to the weak position of the ankle joint with an elevated heel, and a small base of support.
Ankle sprains occur usually through excessive stress on the ligaments of the ankle. This is can be caused by excessive external rotation, inversion or eversion of the foot caused by an external force. When the foot is moved past its range of motion, the excess stress puts a strain on the ligaments. If the strain is great enough to the ligaments past the yield point, then the ligament becomes damaged, or sprained[3][4]
Related Articles:
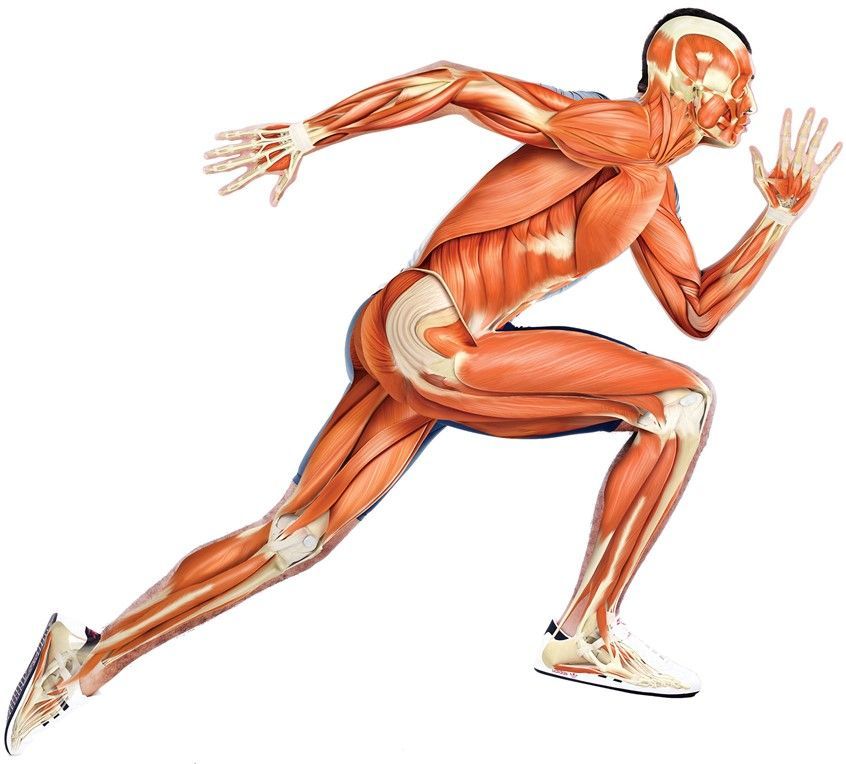
Muscle Strain
(WebMD)
Muscle Strain Overview
Muscle strain — or muscle pull or even a muscle tear — implies damage to a muscle or its attaching tendons. You can put undue pressure on muscles during the course of normal daily activities, with sudden heavy lifting, during sports, or while performing work tasks.
Muscle damage can be in the form of tearing (part or all) of the muscle fibers and the tendons attached to the muscle. The tearing of the muscle can also damage small blood vessels, causing local bleeding (bruising) and pain (caused by irritation of the nerve endings in the area).
Treatment
Our office treats muscle strains using primarily Active Release Techniques to break up adhesions and fibrosis to ensure rapid healing and proper muscle fiber repair in a minimal amount of time. We couple this with flexibility and ultimately strength and stabization of the affected musculature. This allows our patients to resume activity as soon as possible.
Related Articles: