Knee & Leg Pain
General knee pain includes conditions such as runner’s knee, chondromalacia patella,Osgood-Schlatters,etc. These are caused by trauma, or cumulative trauma disorder(overuse).
Causes & Treatment
Most general knee pain syndromes are caused by overuse, and typically occur with a change in shoes, surface, or intensity. Examples would be increasing speed or mileage too quickly for a runner, changing types, styles, or shoe companies, and changing from a treadmill to outdoor surfaces. These variables can all alter biomechanics of the knee joint. Growth spurts while atheletes are maturing, can also alter the mechanics enough to cause one of the above conditions.
Our office works to restore proper mechanics to the knee by focusing on two small typically ignored muscles, first the popliteus, a small muscle in the back of the knee joint, and second the articularis genu, which helps position and stabilize the patella. Active Release Techniques, and sometimes Graston, coupled with flexibility and ultimately a strength and stabilization routine for the quads, hamstrings and lateral stabilizers of the hip and knee gets results where many treatments fall short.
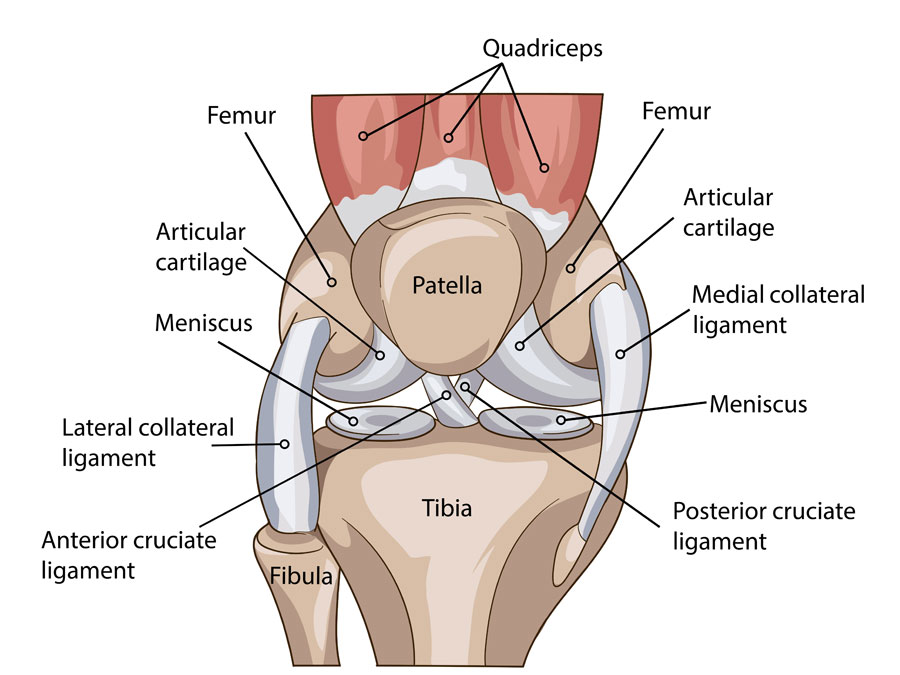
Knee Ligament and Meniscal Pain
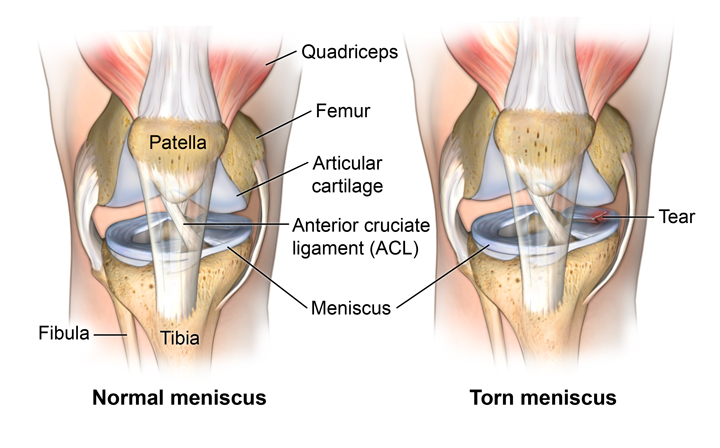
Ligament sprains
Ligaments are strong bands of fascial tissue that connect bone to bone. Ligament sprains are a common injury we see at our office many of these traumas are sports- related. The majority of them are mild to moderate ligament injuries and can be treated conservatively without surgery
An important concept for an injured athlete to grasp is that before one can sprain ligaments, first musculature is damaged trying to prevent damage, then tendons, and ultimately if those two fail, the ligaments can be sprained. This is part of the problem with full immobilization of an athlete, the initial muscular and tendonous damage is not addressed for several weeks, setting the stage for improper healing of the damaged muscles and tendons. This prolongs the time an athlete is out of his or her activity.
Causes & Treatment
Most ligament injuries occur with trauma, and are associated over stretching of the tissues. Meniscal injuries can be due to either trauma or cumulative trauma disorder. After a thorough physical examination and detailed history, the nature and grade of injury to the insulted tissues can be determined. Our office works to restore proper mechanics to the knee by focusing on two small typically ignored muscles, first the popliteus, a small muscle in the back of the knee joint, and second the articularis genu, which helps position and stabilize the patella. If the injured patient is a candidate for conservative treatment, Active Release Techniques, sometimes Graston ,and flexibility and ultimately strength and stabilzation of the surrounding anatomy to support the joint.
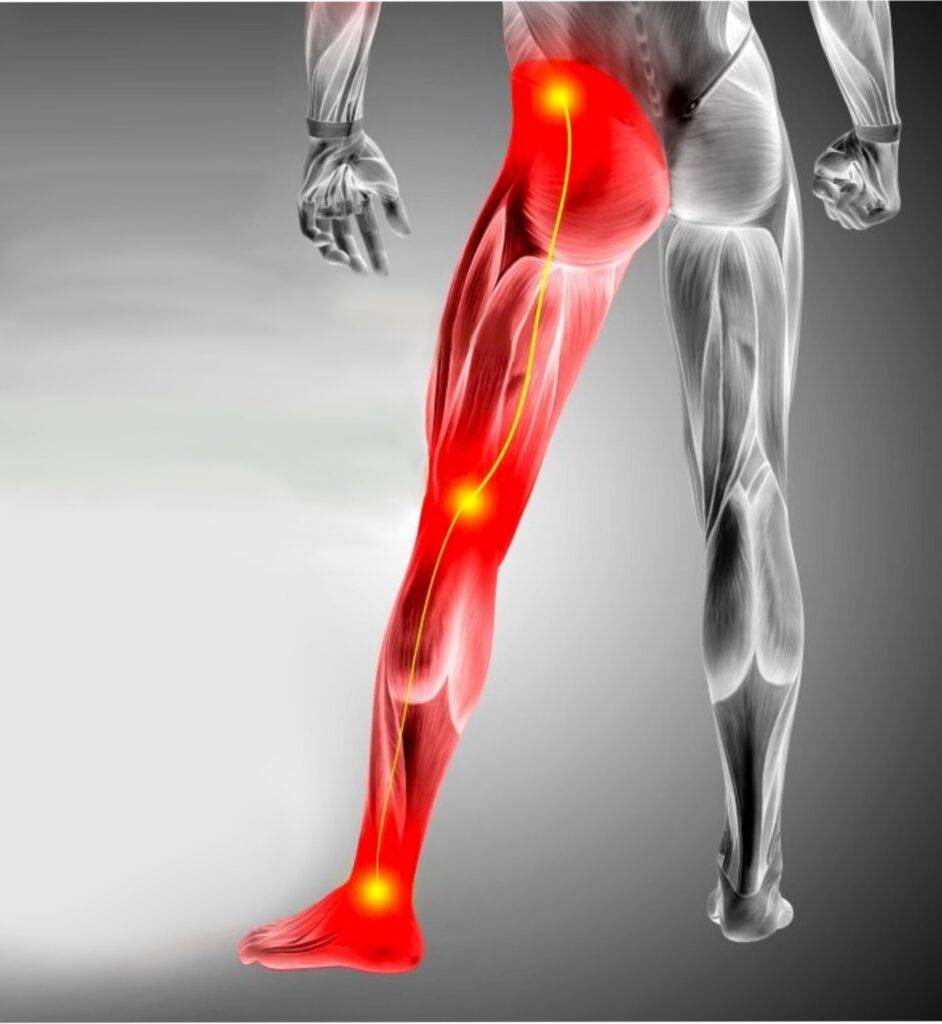
Sciatica
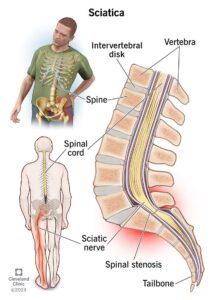
Sciatica is a set of symptoms including pain that may be caused by general compression or irritation of one of five spinal nerve roots, peripheral entrapment by the piriformis, hamstring, calf, or sacral ligaments. Symptoms include lower back pain, buttock pain, and pain, numbness or weakness in various parts of the leg and foot. Typically, the symptoms are only felt on one side of the body, the pain may radiate to the foot, below the knee, or only into the gluteal region.
More accurately, sciatica is a set of symptoms rather than a diagnosis for what is causing the actual pain. The treatment for sciatica or sciatic symptoms differs, depending upon the underlying cause of the pain.
Causes & Treatment
Sciatica can come from numerous causes, from stenosis, to disc herniations, piriformis syndrome, to muscle spasm of the hamstring or gastocnemius with peripheral nerve impingement. A thorough examination and detailed history is essential to differentially diagnosing what is the cause of a patient’s pain.
Our office treats spinal pain using a comprehensive approach, which can include Active Release Techniques, Graston, spinal decompression therapy, spinal manipulation, combined with home stretching and ultimately core stabilization exercises.
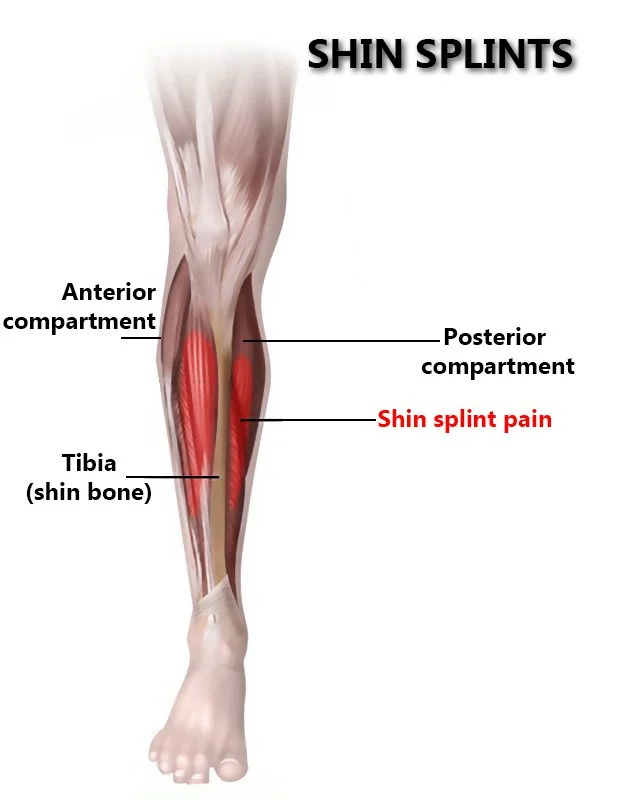
Shin Splints or Compartment Syndrome
(Wikipedia)
Shin splints, known as medial tibial stress syndrome (MTSS), can usually be attributed to overloading the muscles of the lower extremities or to biomechanical irregularities. If an athlete begins running a lot after not running for a long period of time, it puts excess stress on the muscles, causing shin splints. Muscle imbalance, including weak core muscles, can cause lower-extremity injuries, and inflexibility and tightness of the gastrocnemius, soleus, and plantar muscles (commonly the flexor digitorum longus) may contribute, as well.[1] Increasing activity, intensity, and duration too quickly leads to shin splints because the tendons and muscles are unable to absorb the impact of the shock force as they become fatigued; also, the tibial bone-remodeling capabilities are overloaded.
The pain associated with MTSS is caused from a disruption of Sharpey’s fibres that connect the medial soleus fascia through the periosteum of the tibia where it inserts into the bone.[2] With repetitive stress, the impact forces eccentrically fatigue the soleus and create repeated tibial bending or bowing; thus, contributing to MTSS. The impact is made worse by running uphill, downhill, on uneven terrain, or on hard surfaces. Improper footwear, including worn-out shoes can also contribute to shin splints. Risk factors for developing MTSS include:
- Excessive pronation at subtalar joint[3]
- Excessively tight calf muscles (which can cause excessive pronation)[4]
- Engaging the medial shin muscle in excessive amounts of eccentric muscle activity[3]
- Undertaking high-impact exercises on hard, noncompliant surfaces (ex: running on asphalt or concrete)[3]
- Smoker and low fitness [5]
While MTSS is the most common name, other condition often overlap as causes including compartment syndrome and stress fractures. Females are 1.5 to 3.5 times more likely to progress to stress fractures from shin splints.[3][6][7]
This is mostly due in part to females having a higher incidence of diminished bone density and osteoporosis. Shin splint pain is described as a recurring dull ache along the posteromedial aspect of the distal two-thirds of the tibia;[8] the difference in stress fracture pain is that it is typically localized to the fracture site and is more proximal than the pain caused by MTSS.[9]
People with flat feet are especially prone to shin splints.[citation needed] Biomechanically, over-pronation is the common cause for medial tibial stress syndrome.[10] It involves excessive inward rolling that causes tibial twisting and overstretching of the lower extremity muscles. Having poor form, such as leaning forward or backward too much, as well as running with toes pointing outwards all contribute to the causation of shin splints.[citation needed]
Medial tibial stress syndrome is the most prevalent form of shin splints [3] and can affect a broad range of individuals. It affects mostly runners and accounts for approximately 13% to 17% of all running-related injuries.[11][12] High school age runners see MTSS injury rates of approximately 13%.[6] Aerobic dancers have also been known to suffer from MTSS, with injury rates as high as 22%.[13] Military personnel undergoing basic training MTSS injury rates between 4%-6.4%[14] and 7.9%.[15]
Causes & Treatment
Most MTSS and shin splint pain syndromes are caused by overuse, and typically occur with a change in shoes, surface, or intensity. Examples would be increasing speed or mileage too quickly for a runner, changing types, styles, or shoe companies, and changing from a treadmill to outdoor surfaces. These variables can all alter biomechanics of the knee and ankle joints. Growth spurts while athletes are maturing, can also alter the mechanics enough to cause one of the above conditions. When intensity is the culprit, it is an injury of deconditioning. A classic example of this is the first week of track or basketball practice. A change in surface, often shoes, and intensity. The athlete may be quite adequately conditioned for the activity (running), yet not be acclimated or conditioned with regard to the shoes, surface or intensity of the changing sport.
Our office works on getting fluid and swelling out of the affected compartment, so that recovery and healing may occur. We do this through Active Release Techniques, Graston Technique, and effeurage, with conjunction with home cryotherapy and stretching. And ultimately strength, conditioning, and stabilization of the surrounding anatomy.